Fine Needle Aspirates (FNA)
This technique is non-invasive, generally non-painful, quick, and simple. In contrast to histopathology, results are usually available within one working day. FNA is suitable for any surface mass, lymph node or mass in a body cavity that can be palpated and immobilised or aspirated with ultrasound guidance.
Equipment Required
- 3-5 mL or 10-12 mL syringes, 21-23 gauge 0.5-1.5 inch needles. Avoid larger needles as they result in greater blood contamination and “core biopsies” (too thick for cytological examination). Avoid smaller needles as cell lysis may occur.
- Clean glass slides and slide holders for transporting slides
- Pencil for labelling slides in frosted region (permanent marker is removed by the staining process)
- EDTA (lavender top) and plain, non-clot activating (red/lemon top) tubes if fluid is obtained. If there is sufficient fluid, it is always useful to collect samples into both types of tubes. The EDTA sample for cytological examination and the serum/plain tube for culture or other specialized tests (if indicated). An Eswab is preferable for culture.
Collection Technique
- Clipping / shaving of the area is usually unnecessary, but the site should be wiped free of dust and debris
- Localise the mass firmly and stabilise with one hand while sampling with the other using one of the techniques described below.
Aspiration technique – preferred for firm or poorly exfoliating lesions (e.g. mesenchymal neoplasms).
- Insert the needle attached to the syringe into the mass. A larger (10-12 ml) syringe is best for hard lesions. Generally, aspirate from the centre of small masses, but aspirate large masses from periphery, as centre may be cystic or necrotic.
- Apply gentle negative pressure (1/2 – 3/4 volume of syringe)
- Without completely exiting the mass, retract and redirect the needle 3 times with each aspiration attempt (gently releasing suction in between aspiration attempts as the needle is retracted and replaced).
- In most cases, fluid will not be visible within the syringe. The cells are in the needle and hub
- Stop aspiration if any fluid / blood is noted in the syringe (if aspirating a solid mass)
- Release the vacuum before withdrawing out of the body / mass
- Once out of the mass, detach the needle from the syringe
- Draw air into the syringe and reattach the needle
- Gently expel the contents of the needle close to the frosted end of a clean glass slide. If the material is quite liquid, make a smear the same way as for a blood film. For low viscosity fluids, advance the top slide rapidly and lift before reaching the end of the smear. For tacky fluids, advance more slowly. Make several smears if possible.
- If the material is thick, make a squash preparation by gently placing a clean slide on top of the material at right angles or parallel to the other slide.
- Use just enough pressure to smear the material out (often the weight of the slide is enough). Too much pressure will cause cellular disruption
- Pull the second slide along gently until the two slides separate, without lifting the slides directly apart.
- Dry material rapidly with a fan, hair dryer on ‘cool’ setting, or by flapping slides vigorously
Non-aspiration technique – preferred for lymph nodes (neoplastic lymphocytes are quite fragile) or tissues that are more likely to bleed (e.g. thyroid, spleen, etc.). Also may be easier for smaller skin masses, if they exfoliate well.
- Insert the needle into the mass/organ (no syringe attached)
- After redirecting the needle multiple times, withdraw the needle
- Draw air into the syringe and attach to the needle
- Gently expel the contents of the needle close to the frosted end of a clean glass slide.
- Gently place a clean slide on top of the material at right angles or parallel to the other slide.
- Use just enough pressure to smear the material out (often the weight of the slide is enough). Too much pressure will cause cellular disruption.
- Pull the second slide along gently until the two slides separate, without lifting the slides directly apart.
- Dry material rapidly with a fan, hair dryer on ‘cool’ setting, or by flapping slides vigorously
Notes:
- When handling material from aspiration of the lymph nodes and bone marrow, apply as little pressure as possible to spread the aspirated material. Cells are fragile and rupture easily.
- If a bone marrow aspirate is planned, please speak with a Clinical Pathologist prior to sampling for additional advice and information
- When submitting to the laboratory, it is not necessary to fix the smears. It is always a good idea to stain at least one of the smears, and examine to see if there is sufficient intact material on the preparation. Please also submit this smear.
- Prepare a few smears (e.g., 3-4) rather than just one – this allows for examination of more material, and enhances the diagnostic success rate.
- Label smears (with pencil) on frosted end of the slide, on the correct side of the smear, to prevent it from being wiped off in error. (Permanent markers come off in the alcohol used for fixing).
- Send the slides to the lab in slide containers, which are then packaged in bubble wrap to prevent breakage.
Impression smears
These are made when there is a solid piece of tissue available, e.g., biopsy specimen.
- Use a saline moistened swab (sterile saline, not water, as water causes osmotic rupture of cells) to remove superficial debris. If the tissue is bloody, blot with clean paper towel to remove blood first
- Gently touch the surface to a clean slide several times so that there are up to five imprints per slide.
- Dry the slide rapidly by air drying or use a hair dryer on the ‘cool’ setting. This technique can be used for surface lesions but it is not as useful as a FNA for these as the imprint will most often contain just superficial inflammatory cells and the true lesion may not exfoliate.
- NB: If a culture is desired, transport medium can be used to protect swab contents, but once the swab has contacted transport medium that swab cannot be used to make cytology slides.
Scrapings
Some tissues or masses do not exfoliate well on impression smears made from incisional biopsies due to their firm consistency e.g., spindle cell tumours, squamous cell carcinomas, and bone lesions. In cases where impression smears do not result in material on a slide, the scraping technique can provide a diagnostic sample. The cut surface of the tissue is gently scraped with a scalpel blade and the accumulated material is transferred onto a slide and then spread as a squash preparation (see Fine Needle Aspiration section). Dry as above.
Cytobrush Smears
Used for vaginal smears, fistulous tracts, ears, etc. Transfer cells by gently rolling swab along surface of slide.
NB: If a culture is desired, transport medium can be used to protect swab contents, but once the swab has contacted transport medium that swab cannot be used to make cytology slides.
Body Fluids
Cytological examination of body fluids can provide useful information if an organ within the body cavity is diseased. It also helps determine the cause for any increased volume of cavity fluid e.g., ascites. The body fluids most commonly evaluated are pleural, pericardial, peritoneal, cerebrospinal, and synovial. Collection techniques are described in clinical pathology or some internal medicine textbooks.
For all fluids, it is important to:
- Collect most of the fluid into EDTA tubes (lavender top) for cytology, as this prevents clotting and preserves cells to some degree.
- Aseptically place a few drops into a plain serum tube (red/lemon top) or Eswab for culture (EDTA inhibits microbial growth), or use a blood culture bottle.
- Always make a few smears from the fluid immediately after collection. Cells are never as well preserved as when they are first collected.
CSF Collection
For collection techniques, please refer to any recently published anaesthesia or internal medicine textbook.
In small animals, this is generally collected from the cisterna magna, and from the lumbar area in large animals. If a lesion is suspected between the cisterna magna and the lumbar area, then a lumbar puncture is recommended, even in small animals (recognising that this can be difficult to achieve).
CSF Sample Handling
CSF should drip gently from the needle to be collected in a sterile plain (no additive) vacutainer. If a trail of blood appears, discard the first few drops of CSF to collect as clear a sample as possible. If there is sufficient CSF (>0.75 mL), the sample should be aliquoted into 2 red top tubes, one of which will be used for microbiological examination. Alternately, one aliquot can be transferred to a blood culture bottle or Eswab, which is available from Awanui Veterinary.
If the sample cannot be delivered to the laboratory within 30 – 60 minutes, then autologous serum should be added to one of the tubes to preserve cells because they degenerate rapidly due to the low protein content of CSF. EDTA alone is not an adequate preservative.
Procedure for adding protein to CSF (example calculation):
1. The solution should be in a 9 parts CSF to 1 part serum ratio. For example, if you have 1 mL (or 1000 µL) CSF:
Calculation: (90 x 1000 µL)/(100) = Amount of CSF Calculation: (10 x 1000 µL)/(100) = Amount of serum (adjust according volume you have)2. Mix by very gently inverting 5 to 10 times.
Store all CSF tubes at 4ºC and ship (protected by paper towel) on ice. If there will be a very prolonged delay in shipment, make a smear as well. Air dry smears very rapidly using a small fan, hair dryer on “cool” setting, or by flapping vigorously.
Pleural, Peritoneal, Pericardial Fluid Sample Handling
Generally, collecting samples into both an EDTA and a red top (or lemon top) tube is sufficient. Making 1-2 direct preparations of fluid (as you would make a blood film) and air drying rapidly will help the Clinical Pathologist determine things like sampling-associated haemorrhage versus pre-existing haemothorax or haemoabdomen.
Synovial Fluid Collection
Cytological and microbiological examination of synovial fluid is extremely helpful in differentiating septic, immune-mediated, and degenerative joint diseases. As well as in cases of lameness, collecting joint fluid is also useful in cases of pyrexia of unknown origin and in suspected immune-mediated diseases, even in the absence of lameness.
Strict aseptic technique is needed and the necessity for sedation or anaesthesia is dependent on the animal and the joint involved. The carpi and hock joints are commonly affected in immune-mediated diseases.
When collecting synovial fluid, the order of priorities for handling the specimen is:
1. Make 1-2 smears (as you would a blood smear) and air dry rapidly
2. With remaining fluid, place 3-4 drops into blood culture medium or Eswab for possible future microbiological culture. There may be a 50% decrease in the culture rate if the sample is received in a red top container compared with blood culture bottles or Eswabs.
3. Blood culture bottles can be ordered from Awanui Veterinary via our consumables order form.
4. If any fluid still remains, place it into EDTA for cell counts and assessment by the clinical pathologist
Nasal Cavity Sampling
It may be difficult to get a diagnostic sample from a suspect lesion in the nasal cavity. Nasal swabs often do not yield satisfactory material as they cannot be inserted far enough or are not abrasive enough to yield representative samples of deep mucosal lesions. Submitting the exudate also usually gives non-specific results. A diagnosis may occasionally be obtained if a causative agent such as Cryptococcus is present. A cytobrush, direct aspiration or a squash smear from a biopsy can be used to obtain diagnostic material from deeper lesions.
NB: If a culture is desired, transport medium can be used to protect swab contents, but once the swab has contacted transport medium that swab cannot be used to make cytology slides.
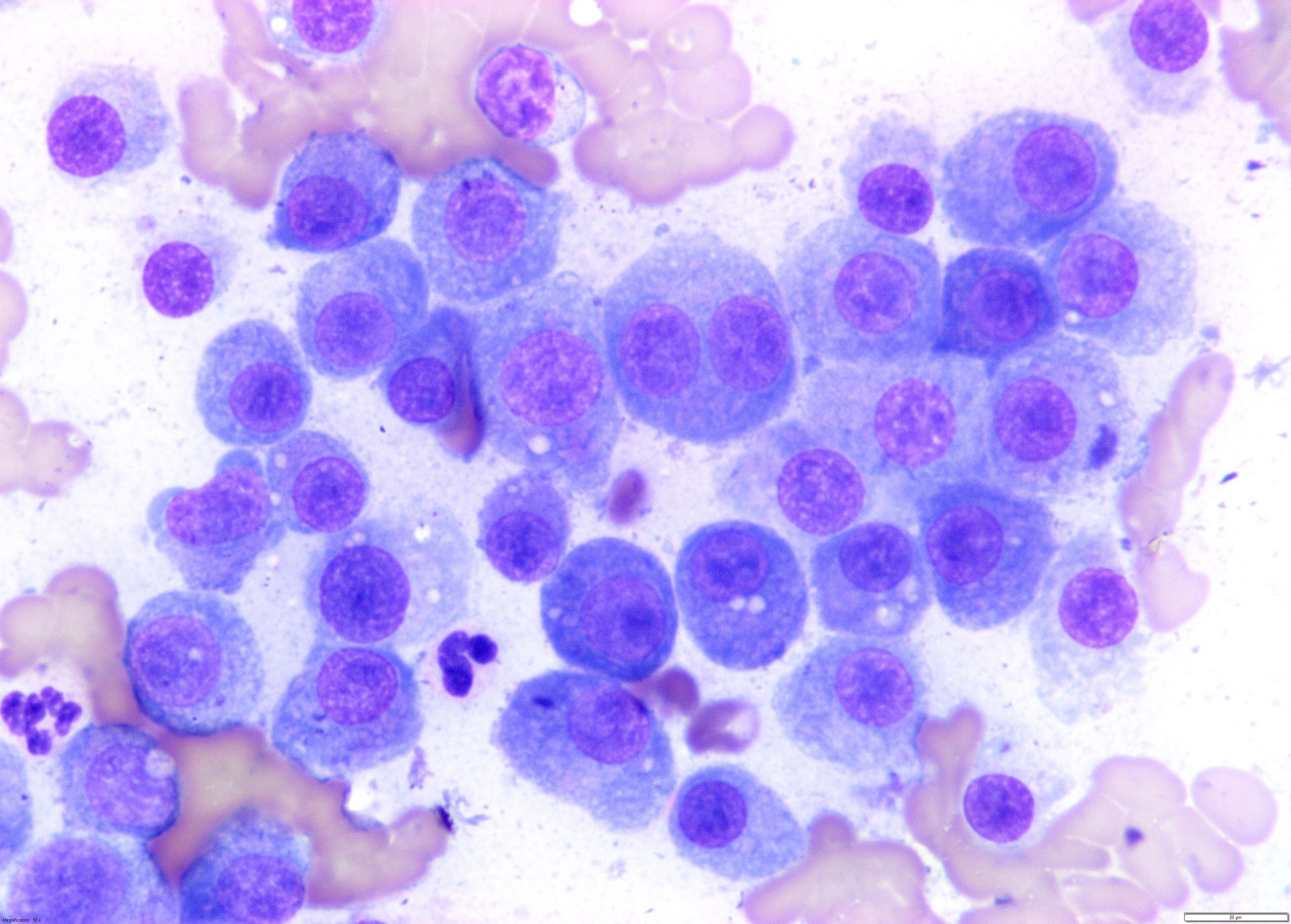
Bone Marrow Examination
Examination of bone marrow is an adjunct to haematology and is indicated in a number of different circumstances. These include:
- Pancytopenia (anaemia + neutropaenia + thrombocytopaenia) or bucytopaenia
- Persistent, unexplained, non-regenerative anaemia
- Persistent, unexplained neutropaenia with no left shift
- Persistent, unexplained thrombocytopaenia (rule out DIC first, can perform even with platelets as low as 10 x109/L, tends not to cause problems so long as secondary haemostasis is adequate)
- Leukocytosis, especially if there are atypical cells in the blood
- Atypical cells or immature cells
- Hyperproteinaemia due to a monoclonal gammopathy (or polyclonal if ehrlichiosis is a possibility due to travel history of the animal, but assess lymph nodes first)
- Hypercalcaemia with no other identifiable cause
- Pyrexia of unknown origin
- Clinical staging of neoplasia
- Evaluation of iron stores (not in horses, cats, neonatal animals)
Bone Marrow Aspiration – Dogs, Cats, Horses, Cattle
As with all of these techniques, a good, current internal medicine textbook will have all the information you require for obtaining bone marrow cores and aspirates, but following are a few extra points and tips. A concurrent CBC is required for a proper assessment of bone marrow. Bone marrow core biopsies and cytology very much complement one another. Individual cell morphology is largely a mystery on histology, so that is why cytology is required.
- Consider adding sodium bicarbonate to the lidocaine (immediately prior to injection) to minimize pain (e.g., 0.9 mL lidocaine and 0.1 mL sodium bicarbonate. Do not increase sodium bicarbonate beyond 10% as this will cause precipitation of lidocaine, mix immediately prior to use).
- “Rinsing” the syringe(s) to be used for aspiration with sterile EDTA can help prevent clotting (take up some sterile EDTA and expel it, enough will remain in the syringe).
- Syringe contents can be placed in an EDTA from which excess EDTA has been shaken out and submitted to the laboratory as is, or expelled onto a petri dish held at an angle to drain off excess blood. Individual particles can be suctioned up using a pipette, transferred to a glass slide, from which pull apart smears can be made. Otherwise, excess blood can be allowed to drain down a glass slide and then a squash preparation can be made. Finally, a regular “blood film making” technique can be used to make both feather edge and “stop edge” preparations. The latter involves stopping the pushing slide so a line of material results. This concentrates cells of interest and minimises breakage that can occur with the feather-edge preparation technique.
- Dry slides rapidly with a small fan, a hairdryer set on “cool”, or by flapping vigorously.
- It is good to stain one in house and and examine microscopically to ensure adequate cellularity.
- Please remember to package the bone marrow core in formalin separately from cytology slides – formalin alters the cells and sometimes ruins the sample completely.